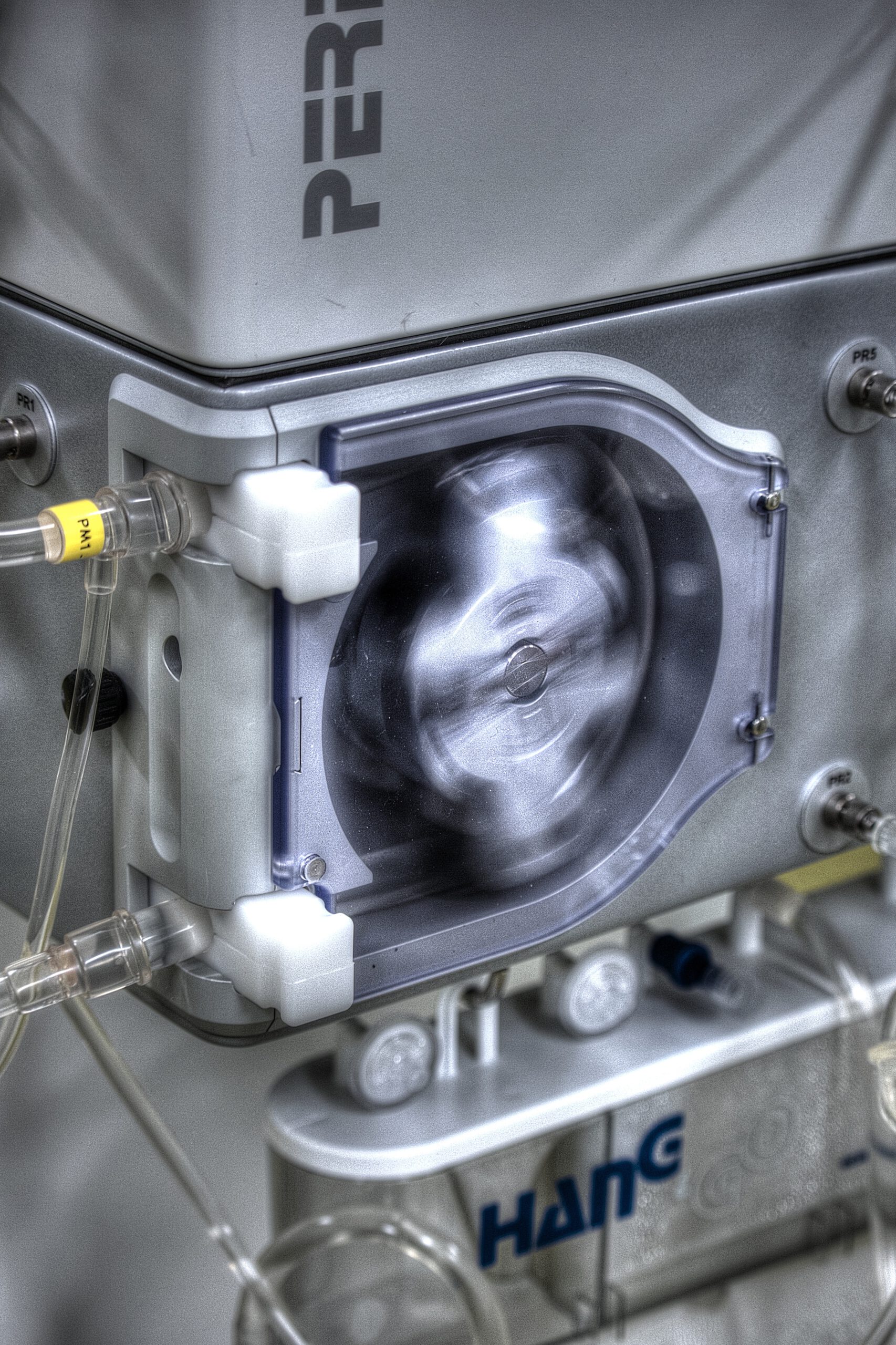
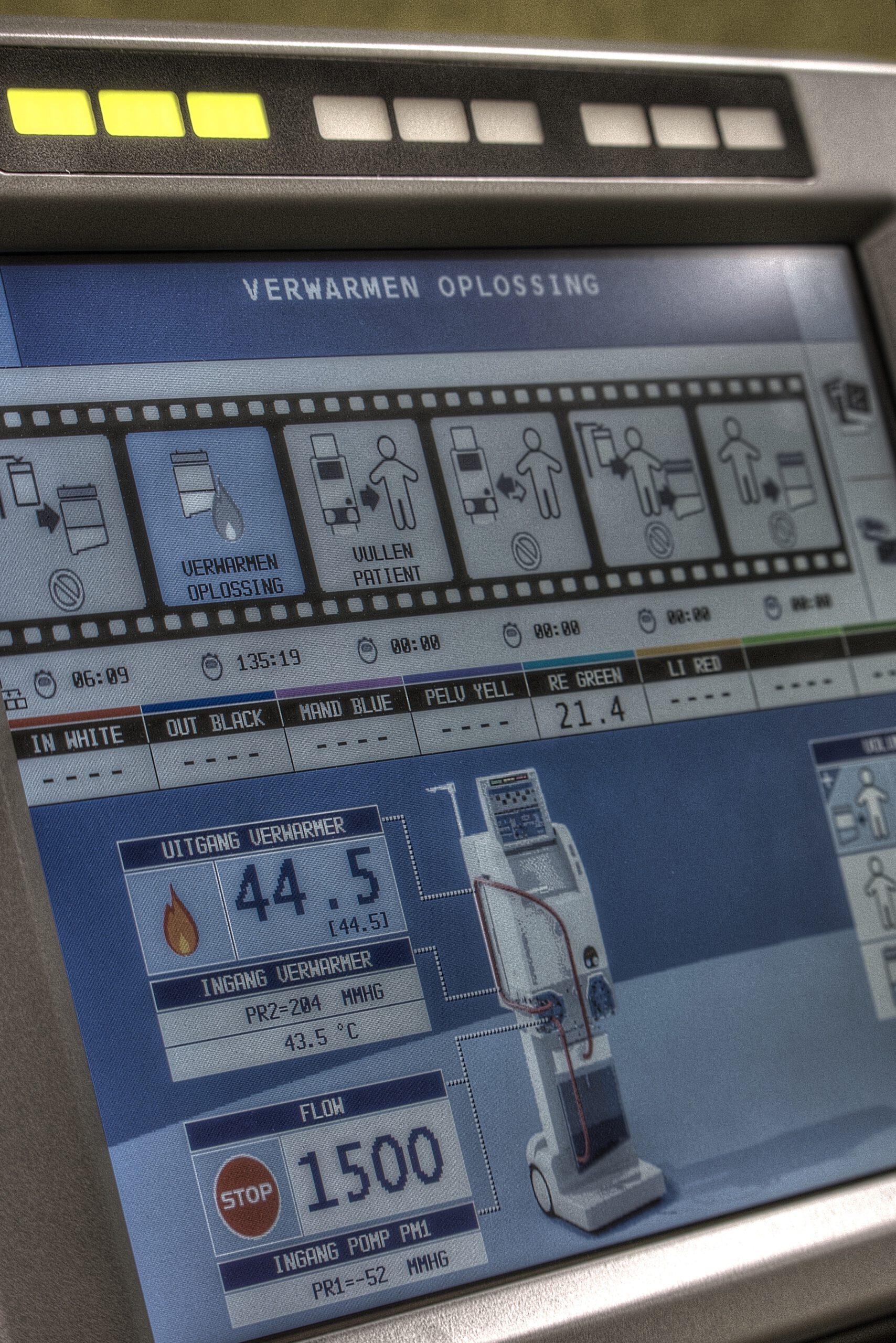
Hyperthermic Intra Peritoneal Chemotherapy (HIPEC) delivers heated chemotherapy at a temperature of 41-43 C (105-109 F) to the abdominal contents for 90 minutes. Prior to the treatment it is necessary to surgically excise all visible tumor to a minimum size of 3mm.
Better equipment and disposables leads to improvement of treatments
Better training and deployment of specialized personnel leads to better results
Combining treatments
Recurrent ovarian, primary peritoneal and Fallopian tube cancers and endometrial cancer tend to stay within the abdominal cavity and adjacent lymph nodes for relatively long periods of time. This means that they should be amenable to a combination of surgery together with intraperitoneal chemotherapy.
Interesting…
The technique was originally described for the treatment of patients with advanced gastric and colorectal cancers but has intriguing possibilities in ovarian, primary peritoneal, Fallopian tube and endometrial cancer and to date little has been reported on the subject.
Intra peritoneal delivery of chemotherapy agents has an established record in ovarian cancer and current evidence suggests that there is a disease free survival advantage for patients receiving chemotherapy in part by this route.
Since with HIPEC adhesions are divided at the time of surgery there is theoretically an improved distribution of drug through the abdominal cavity.
The combination of chemotherapy with heat is thought to work because the heat encourages greater uptake of the agent into tumor cells and the combination may reverse chemotherapy resistance.
In addition, heat itself at the temperatures used, 41-43 C, (105-109 F) has been shown to be tumoricidal.
The heated chemotherapy treatment itself is well tolerated. It is necessary to ensure a good urine output during and following the surgery and there may be a slightly increased risk of complications following bowel surgery.



